Resistance Guided Therapy
The misuse and overuse of antibiotics has impacted their effectiveness globally. Diagnostics that detect infection and genetic markers for antibiotic resistance in a single test enable you to implement Resistance Guided Therapy (RGT). Utilising an RGT approach is clinically demonstrated to improve patient cure rates1 and is recommended by international bodies as the preferred method of treatment for infections such as Mycoplasma genitalium (Mgen) or gonorrhoea.2-6
Why is Resistance Guided Therapy important?
- Improve patient treatment outcomes
- Reduce re-admission and healthcare costs
- Minimise the spread of antibiotic resistant infections
- Maintain the efficacy of antibiotic treatment (antibiotic stewardship)

Resistance Guided Therapy Improves Patient Experience
Watch the video to learn about Chris and Luke: two patients who contracted Mycoplasma genitalium infections but with very different personal stories.
Without access to RGT, Luke experienced delays in diagnosis and incorrect treatment regimes which resulted in extended time living with uncomfortable symptoms.
Chris was able to access RGT at his first clinic visit. His Mgen test result indicated he had a resistance infection so he received the appropriate second-line treatment straight away, reducing his time to cure.
RGT can positively impact patient outcome while reducing overall healthcare costs associated with return patient visits and failed treatments.
Resistance Guided Therapy dramatically improves cure rate
Resistance Guided Therapy achieves better cure rates for Mycoplasma genitalium (Mgen)
Cure rate of Mgen without RGT
Cure rate of Mgen with RGT
Reference: Read TRH et al. Clinical Infectious Diseases 2019; 68(4):554-560
Case Studies
Guidelines for management of infectious diseases are moving away from empiric treatment pathways towards more directed use of antibiotics. Following RGT practices can positively impact patient cure rates while reducing overall healthcare costs.
Resistance Guided Therapy for Mgen
Data from Melbourne Sexual Health Centre demonstrated successful increase in cure rate when using RGT compared with previously used Mgen-detection only approach. Substituting azithromycin with doxycycline for empiric treatment, with subsequent treatment of Mgen infections based on resistance result, cure rates increased from below 67% to ≥92%:
- Differential treatments based on the results of the ResistancePlus® MG test resulted in a cure rate of ≥92% of infections, with infrequent selection of macrolide resistance.
- Previous cure rates from the clinic population exhibiting high levels of antibiotic resistance have been reported below 67% and as low as 40% when treating with standard front-line azithromycin therapy.
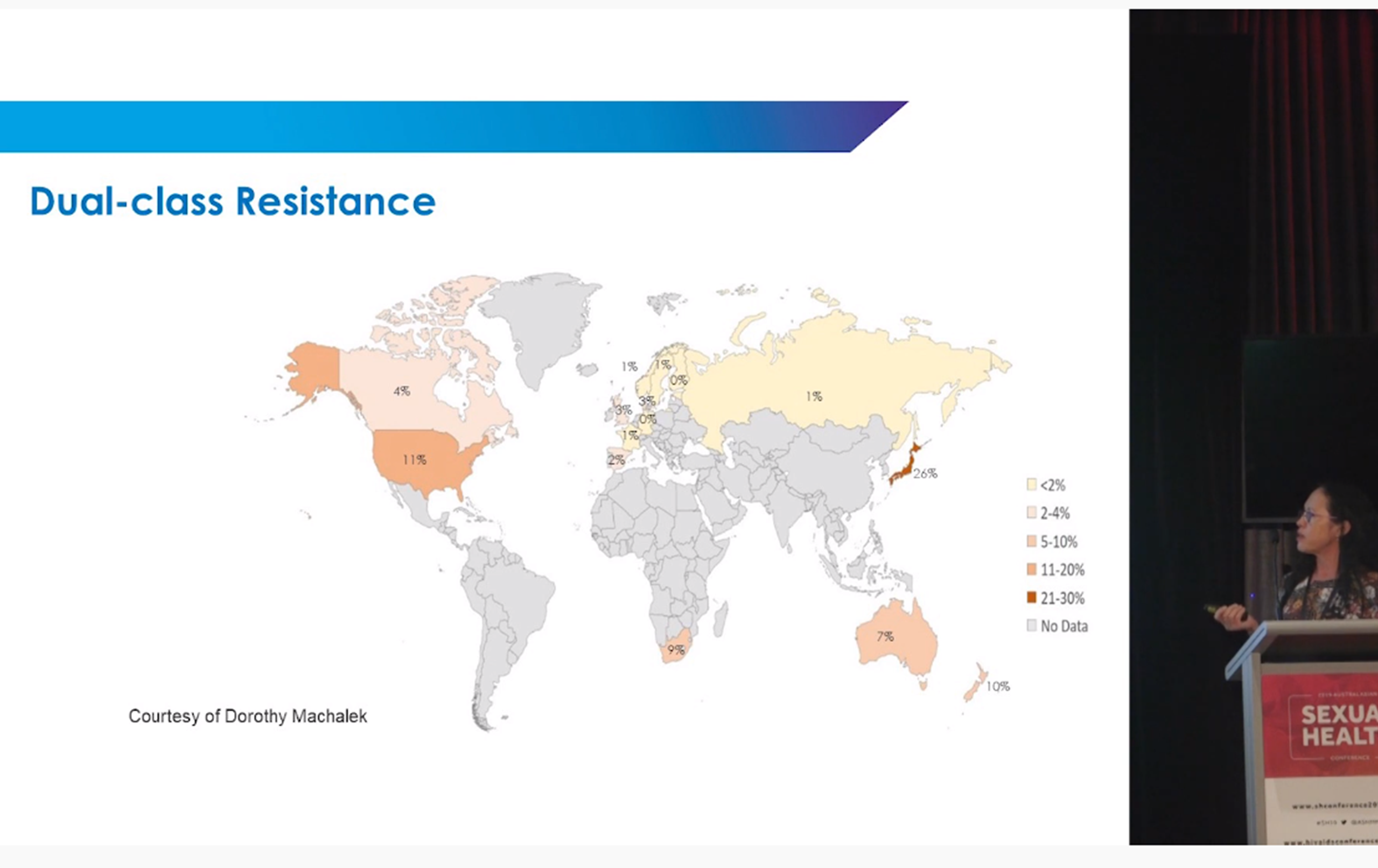
Resistance Guided Therapy for gonorrhoea
Action is urgently needed to improve the management of gonorrhea, including strategies to preserve the efficacy of ceftriaxone, one of the last remaining antibiotics available for multi-drug resistant infections. Surveillance data indicates that in some regions up to 7 out of 10 infections could be effectively treated with a single, more convenient oral dose of ciprofloxacin if the susceptibility status is established prior to prescribing.
- Targeted therapy based on RGT approaches can reduce the use ceftriaxone, a painful intramuscular injection.
- Guidelines are moving towards preferential use of ciprofloxacin if susceptibility status of infection is determined prior to treatment.*
*Recommendations by British Association of Sexual Health and HIV (BASHH).
Publications and Media
We are committed to supporting continued scientific discovery and generation of clinically relevant data. Collaborations with key researchers and clinicians around the globe help us improve diagnostics and address urgent clinical needs.
The Value of Molecular Tests to Diagnose and Detect Ciprofloxacin Susceptible Gonorrhoea in Clinical Practice
Provides background on gonorrhoea treatment options and speaks about the clinical utility of Resistance Guided Therapy in the context of ciprofloxacin susceptibility testing when treating gonorrhoea.
Evolution of Resistance Guided Therapy
Discussion on the value of Resistance Guided Therapy in the clinic, including experiences of early access to ResistancePlus® MG FleXible – near patient macrolide resistance testing for Mgen infections – and the expected impact of near-patient testing.
Outcomes of Resistance-guided Sequential Treatment of Mycoplasma genitalium Infections: A Prospective Evaluation
Read TRH et al. Clinical Infectious Diseases, Volume 68, Issue 4, 15 February 2019, Pages 554–560.
The seminal publication demonstrating significant improvements to Mgen infection cure rate through the use of doxycycline for emperic treatment and implementation of ResistancePlus® MG to guide subsequent treatment decisions. Cure rates improved from below 60% to over 92%.

