Testing
Confident SARS-CoV-2 Testing
The PlexPCR® SARS-CoV-2 assay can help your laboratory regain efficiency through pandemic and post-pandemic testing. Based on our PlexZyme® technology, targeting highly conserved regions (RdRP/ORF1ab), and with automation compatibility – your laboratory can easily stay on top of COVID-19 testing and the supply challenges the pandemic has brought.
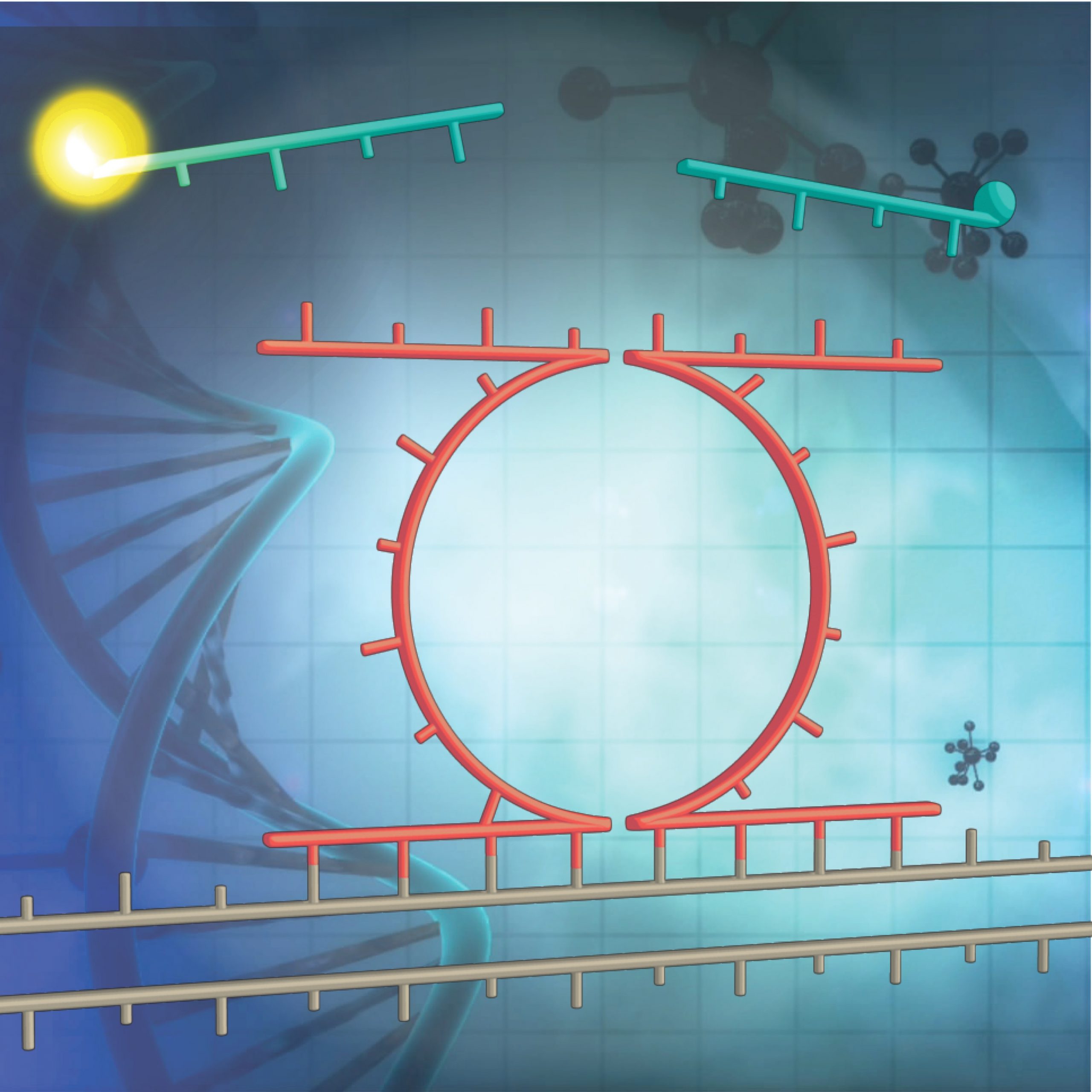
Secure supply chain with PlexZyme® Technology
Effective COVID-19 management is dependent on reliable and frequent testing. Disruptions in global manufacturing supply chains continue to limit availability of laboratory diagnostic kits, impacting local testing strategies.
SpeeDx utilises PlexZyme® technology, de-coupling the detection probe from the primer sequence to produce universal probes. These probes are used across our entire product portfolio, enabling production and stockpiling of the probes well in excess of ‘market demand’ to negate any impact from supply chain constraints. This enables us to manufacture and readily ship kits in high volumes at all times – ensuring no interruptions to your daily laboratory testing. Learn more.
Confident SARS-CoV-2 testing
SARS-CoV-2 continues to mutate, giving rise to variants potentially impacting diagnostic testing and reporting. Reliable and accurate diagnostics are required by laboratories to save time, resources, and to have confidence in the data reported.
SpeeDx routinely monitor the performance of our PlexPCR® SARS-CoV-2 assay against emerging variants to ensure your laboratory can continue to report patient test data with no hesitation. Learn more.
Resistance Guided Therapy
SpeeDx ResistancePlus® diagnostics detect the infecting organism and antibiotic susceptibility or resistance markers – empowering clinicians to make informed patient treatment decisions.
What is Resistance Guided Therapy?
Resistance Guided Therapy (RGT) uses advances in diagnostic technology to help clinicians choose the best targeted therapy for individual patients based on the resistance status of their infection.
- RGT uses tests that detect the infecting organism and genetic markers linked to antibiotic susceptibility or infection
- RGT can replace empiric treatment models by providing additional information at the time of diagnosis to guide appropriate treatment decisions
Why is Resistance Guided Therapy important?
Strategies for controlling many STIs are dependent on the availability of inexpensive yet highly effective antibiotics. As antimicrobial resistance rates rise in these infections it is even more important to use our limited antibiotics more wisely.
Guidelines for management of STIs caused by Mycoplasma genitalium and Neisseria gonorrhoeae increasingly recommend RGT to help:
- improve likelihood of effective patient treatment
- reduce re-admission and healthcare costs
- minimise the spread of antibiotic resistant infections
- maintain the efficacy of antibiotic treatment (antibiotic stewardship)
Declining cure rates when employing detection-only practices for M. genitalium addressed with implementation of RGT, increasing cure rates for macrolide susceptible populations to 95% and total population cure rate over 92%.1
Resistance Guided Therapy
Improve cure rate and simplify patient management.
Implement RGT in your Laboratory
ResistancePlus® tests give your laboratory a competitive advantage. Now you can offer your clinicians more than just detection. The combination of resistance data with infection detection in a single-well test, enables RGT for improved patient management.
Products
ResistancePlus® tests combine organism detection with genetic markers linked to antibiotic susceptibility or resistance. PlexPCR® tests combine multiple, clinically relevant infectious disease targets into a single test solution.
Sexually Transmitted Infections
ResistancePlus® GC
Single well qPCR test detecting Neisseria gonorrhoeae and markers linked to ciprofloxacin susceptibility
PlexPCR® VHS
Single well qPCR test detecting and differentiating HSV-1, HSV-2, VZV & Treponema pallidum (Syphilis)
ResistancePlus® MG
Single well qPCR test detecting Mycoplasma genitalium and markers linked to macrolide resistance
PlexPCR® HSV-1&2, VZV
Single well qPCR test detecting and differentiating HSV-1, HSV-2 and VZV
Respiratory
PlexPCR® RespiVirus
2 well qPCR test detecting and differentiating 11 respiratory viruses
GeneXpert®
ResistancePlus® MG FleXible
Cartridge-based test detecting M. genitalium and macrolide resistance markers
Discover More

Workflow Solutions |
Resistance Guided Therapy |
Technology |
Collaborations |

Publications & Media |

Conferences & Events |
Deliver innovative clinical diagnostics to improve patient outcomes
Latest News
About SpeeDx
Our mission is to deliver innovative clinical diagnostics to improve patient outcomes. Meet the SpeeDx Team, learn about our key collaborations and partnerships, and join our passion to change the face of diagnostics.
References:
1Read TRH et al. Clinical Infectious Diseases 2019; 68(4):554-560
2Harris SR et al. Lancet Infect Dis Published online May 15th 2018
3Lahra MM et al. Australian Gonococcal Surveillance Programme annual report, 2015
4Heffernan H et al. Antimicrobial resistance and molecular epidemiology of gonococci in NZ, 2014-5
5Kirkcaldy RD et al. MMWR Surveillance Summaries July 15, 2016 / 65(7);1–19
